Bridging the gap in health: Addressing inequity of HIV and mental health epidemics among men who have sex with men in the Philippines

Author(s)/Editor(s): Aron Harold G. Pamoso, Mary Lou Rasmussen, I Nyoman Sutarsa, Brett Scholz
Publication year: 2025
Publication type: Policy Brief
EXECUTIVE SUMMARY
The Philippines has witnessed a significant increase in HIV cases, marking the highest rate in the Western Pacific Region. Men who have sex with men in the Philippines are particularly hard hit, representing a large portion of the rising HIV population. In addition to the challenges related to HIV, these men, regardless of their HIV status, often struggle with mental health issues. The intersection of these health problems creates a compounded effect, influenced by various structural, political, and cultural factors that contribute to their marginalization. This policy brief highlights how using critical frameworks—intersectionality and syndemics—can empower stakeholders, including policymakers and healthcare providers, to create holistic, meaningful, and culturally appropriate interventions and policies. It also discusses the importance of democratizing expertise through leadership from those with lived experiences, which can aid in developing culturally informed policies and interventions. Recommendations are included.
INTRODUCTION
It has been over four decades since the world first encountered HIV, and today, we can see how medical advancements have saved millions of lives, transforming HIV from a life sentence into a condition that allows people to live fulfilling lives to the fullest. This positive trend is evident in countries like Australia, where the number of new HIV notifications has decreased in recent years. However, the success in mitigating HIV varies across countries. In particular, the Philippines has experienced the highest number of new HIV cases in the Western Pacific Region, with a 174% increase in incidence from 2010 to 2017. To put this in context, from 2013 to 2023, there has been a reported 411% rise in daily cases over ten years.
Since 1984, there have been 143,778 reported cases of people living with HIV under the HIV & AIDS Surveillance of the Philippines. According to a recent report from the Epidemiology Bureau of the Department of Health of the Philippines, there were more than 47 new cases of individuals living with HIV reported from October to December 2024, bringing the total to 4,245 newly reported cases. Unprotected sex remains the leading cause of HIV transmission. In the last quarter of 2024, 4,050 people acquired HIV through sexual contact, accounting for 96% of the total. Of these, 2,973 were male-to-male, 563 were male-to-male/female, and 514 were male-to-female.
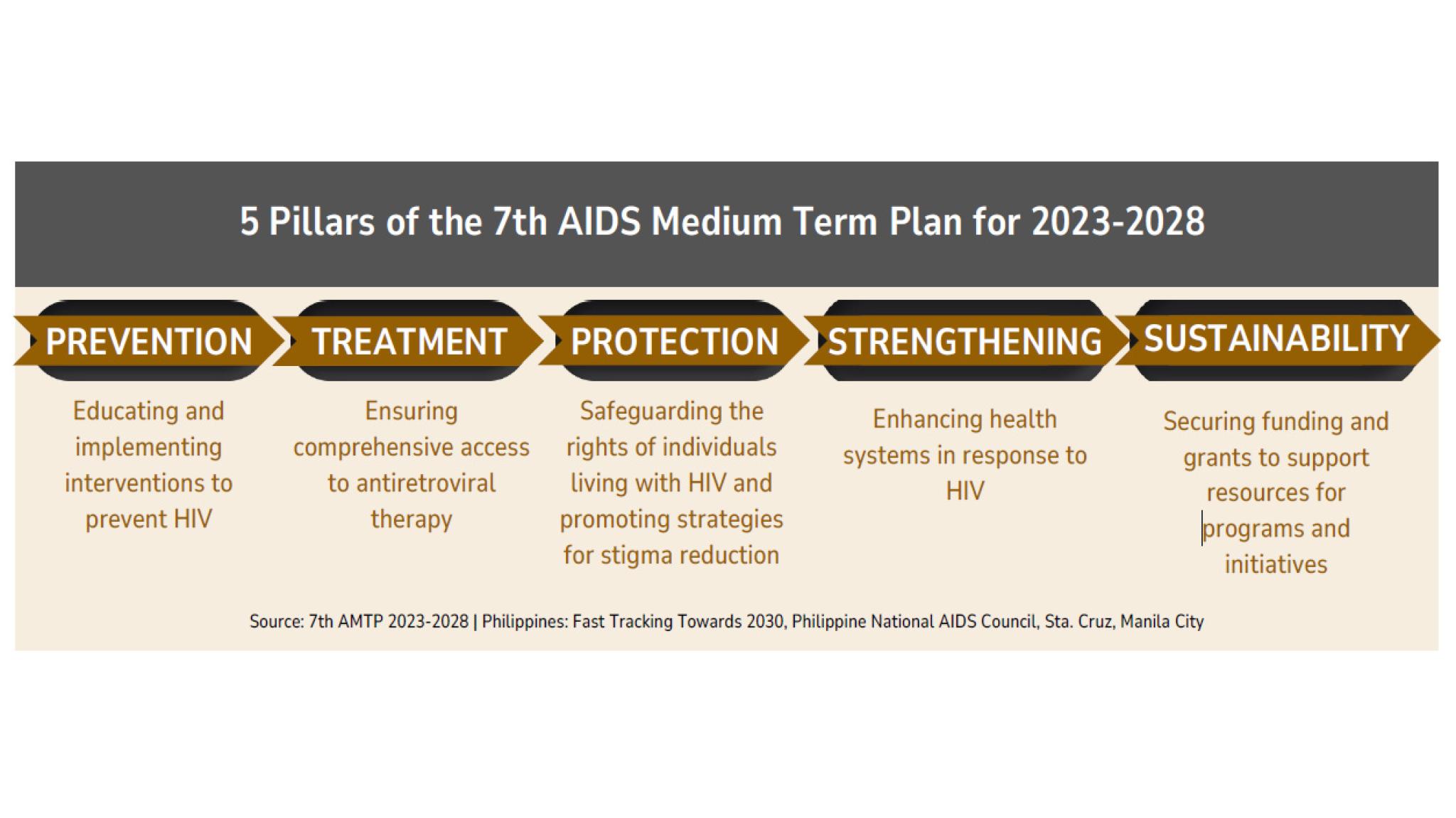
In addition to their sexual health challenges, these men, regardless of their HIV status, are also confronted with ongoing mental health issues. Extensive literature indicates that sexual and gender minorities, particularly men who have sex with men, experience poorer mental health compared to their straight counterparts. In our previous work, we outlined evidence demonstrating how this population grapples with ongoing mental health struggles and how their sexual health, specifically their HIV status, is interconnected with their mental health. Filipino men who have sex with men are stigmatised because their sexuality, for being gay or bisexual, does not conform to the traditional values of the Philippine society. When these men are living with HIV, they also face stigma because living with HIV is seen as sinful and immoral in Philippine society. Such experiences of marginalisation may lead to poor mental health outcomes for these men.The global community, in partnership with the Joint United Nations Programme on HIV/AIDS (UNAIDS), has established the 95-95-95 targets. These targets commit to ensuring that by the year 2030, 95% of individuals living with HIV will be aware of their status, 95% will be receiving antiretroviral therapy, and 95% will achieve viral suppression. In the Philippines, the government has instituted the Philippine National AIDS Council to combat the HIV crisis within the nation. They have developed the framework known as the 7th AIDS Medium Term Plan for the years 2023-2028, which aspires to eradicate AIDS in the Philippines by 2030. This framework is comprised of five pillars: 1) Prevention: Educating and implementing interventions to prevent HIV; 2) Treatment: Ensuring comprehensive access to antiretroviral therapy; 3) Protection: Safeguarding the rights of individuals living with HIV and promoting strategies for stigma reduction; 4)Strengthening: Enhancing health systems in response to HIV; 5) Sustainability: Securing funding and grants to support resources for programs and initiatives.
Addressing the rapid growth of people living with HIV is a governmental priority in the Philippines. Actions have been taken, such as the implementation of the HIV cascade through various mechanisms, including HIV testing, counseling, monitoring, antiretroviral therapy, pre-exposure prophylaxis (PrEP), and post-exposure prophylaxis (PEP). In particular, healthcare workers, such as doctors, nurses, and counselors, have demonstrated knowledge of PrEP and PEP. However, they emphasize the limited resources available for delivering these interventions to target populations. Similar sentiments have been observed among Filipino men who have sex with men. In terms of HIV testing, self-testing has shown high engagement within this population. Yet, they have reported similar concerns regarding infrastructure. Currently, HIV cascade services, including testing, PrEP, PEP, and antiretroviral therapy, remain freely accessible to key populations, including men who have sex with men.
But why, despite the availability of resources and interventions, do we still see an increase in new HIV cases and poor mental health outcomes within this population? In our prior work, we argued that understanding these two health conditions, HIV and mental health, requires going beyond biomedical approaches. It necessitates a deeper examination of how structural forces, such as political and cultural dimensions, shape these health conditions and the experiences of men who have sex with men. This nuance and exploration provide insight into how stigma rooted in cultural, social, and political elements influences HIV and mental health of this population.
Our study found that gay and bisexual men living with HIV in the Philippines face multiple layers of stigma. They experience discrimination not only because of their HIV status but also due to their sexuality. This stigma is often reinforced by conservative religious beliefs and family structures, pushing them further to the margins of society. Our research raises questions about how health issues in this group can be better understood and how structural and political factors shape their experiences.
A recent academic essay highlighted the dual epidemics faced by Filipino men who have sex with men, including gay and bisexual men. Scientific evidence shows that this population experiences overlapping health challenges related to HIV and mental health, compounded by cultural and political factors that contribute to their marginalisation. The essay emphasised the need for policymakers, healthcare workers, and community members to take a holistic approach to addressing these issues.It recommended using critical frameworks such as syndemics and intersectionality. Syndemics examines how multiple health issues interact and worsen within specific groups, while intersectionality helps explain how overlapping social identities can lead to marginalisation and oppression. In this context, factors like HIV-related stigma and heterosexism further shape the experiences of Filipino men who have sex with men.
Integrating these two theories into the understanding of the marginalization faced by Filipino men who have sex with men, including gay and bisexual men, will help stakeholders gain a holistic view of the health challenges these men face (regardless of the HIV status and mental health condition)—particularly regarding HIV and mental health—while also understanding how cultural and political structures in the Philippines fuel their marginalization.
We have listed recommendations below on how to address the HIV and mental health issues faced by Filipino men who have sex with men.
RECOMMENDATIONS
Incorporating lived experiences and affected communities in healthcare and policy-making
To integrate the lived experiences of Filipino men who have sex with men and their communities affected by HIV and mental health issues, we need to create HIV and mental health programs and initiatives that authentically align with their experiences, valuing them as experts in these health conditions and utilizing their experiential knowledge to guide and inform policies. Doing so will foster a commitment from the government and health systems to involve this population and their communities meaningfully.
Addressing the HIV and mental health issues in this population requires reforms at both the healthcare and policy-making levels. The inequities experienced by these men arise from power imbalances between the marginalized group—men who have sex with men—and the decision-makers regarding their health, specifically, the policymakers who create legislation and frameworks for implementing HIV and mental health systems, as well as the society at large that views them as ‘different’ compared to the general population. Instead of perceiving these men as victims, we need to create opportunities for them to grow and thrive, empowering them to become leaders. This shift from victimhood to leadership will cultivate an environment where these men are empowered to leverage their experiential expertise and lived experiences to inform both health systems and policymaking, fostering a system that recognizes them as experts, leaders, and agents of change.
The authentic representation of these men’s lived experiences in health systems will not be possible without reforms in policymaking. Regardless of our efforts to engage this population for authentic representation in HIV and mental health systems, without policy reforms, achieving genuine representation remains unattainable. For example, creating HIV and mental health interventions and programs that utilize the lived experiences of these men will not be entirely feasible without adequate resources and funding. Often, these resources and funding result from effective policymaking and implementation. Therefore, we assert that to authentically represent the lived experiences and expertise of these men in driving change in the HIV and mental health systems, policymakers must genuinely involve them in the policy-making process. To achieve the first recommendation, Filipino policymakers should authentically engage the community, including men who have sex with men and other marginalised groups, in designing and implementing HIV and mental health programs and initiatives while ensuring adequate funding and legal protections. With the support of the Australian government, they can collaborate through strategic partnerships, financial assistance, and capacity-building initiatives.
Greater involvement of community-based organizations in the HIV and mental health response
To achieve greater community involvement in addressing HIV and mental health issues, policymakers and healthcare systems must strengthen their partnerships with affected communities by treating them as equal partners. This collaboration fosters a multisectoral response to HIV and mental health epidemics aimed at creating holistic interventions and programs.
We have acknowledged that the current health systems in the Philippines are responding to calls for action regarding the ongoing problems of HIV and mental health. For instance, the national health insurance of the nation — Philippine Health Insurance Corporation (PhilHealth)—has expanded its outpatient HIV treatment benefit and created an outpatient mental health benefits package. Although there have been reforms in tackling HIV and mental health problems, access to sexual and mental health services remains inaccessible. This is an opportunity for various community-led organizations to augment the limited resources available. For example, we assert that community-based and community-led organizations tackling HIV and mental health present opportunities where they can showcase their lived experience leadership and provide authentic representations of their lived experiences in health reforms and policies. These institutions stand at the forefront in demonstrating that lived experience leadership is a key strategy in addressing the ongoing challenges faced by people with stigmatized social identities and health conditions. Organizations such as Lived Experience Australia demonstrated how to authentically engage people with lived experience of mental health conditions in advocacy, research, program initiatives, and policy making.
Aside from prioritizing the national and local health systems in the Philippines, the government will also leverage various community-led and community-based organizations in addressing HIV and mental health issues among these populations. Various scientific literature has noted the positive impact of grassroots and community-based organizations and interventions in tackling these health problems. If a positive impact has been observed with community-led and community-based interventions, how much more could be achieved if such initiatives are backed and partnered with the government?
Increasing Government support by allocating resources for expanding the programs’ reach
Resources are essential for the creation, development, and implementation of responses to HIV and mental health challenges. The governments of Australia and the Philippines, in conjunction with other funding agencies, must strengthen their commitments and partnerships to guarantee that resources and funding for HIV and mental health interventions are readily accessible to those in need populations.
Australia has been recognized as a leader in HIV response. Recently, the Australian government has formed partnerships with UNAIDS to boost its HIV response. The funding agreement aims to foster HIV responses among various governments and communities to improve their HIV response over the next four years. This is great news, as it shows the Australian government's commitment to the global community in ending AIDS by 2030.
The response to both HIV and mental health epidemics requires thorough resources and equitable access to such resources. The backbone of various HIV and mental health responses and initiatives comes from various funding opportunities. However, we also cannot deny that the forefront of HIV and mental health responses comes from various community-based and led initiatives.
Community-based and grassroots initiatives play a crucial role in HIV and mental health responses. Organizations like AIDvocates lead efforts at the community level by providing HIV testing, counseling, and education. These initiatives are often sustained through the dedication of community volunteers, who support their work through fundraising and other resource-generating activities. Moreover, the first author of this policy brief also had the opportunity to connect with Filipino gay and bisexual men living with HIV and found that they financially contribute to each other so they can afford to seek mental health professionals for therapy and counseling. From these examples, we know that the community has the motivation and passion to deliver help to its fellow members. However, we cannot overlook the fact that resources remain scarce, which may lead to inaccessibility to quality services.
Addressing this problem requires an overhaul of the systems and policies, which we believe necessitates immense resources and time. Policymakers and the government can start involving more community members in their policy-making initiatives while authentically engaging with them.
The current political landscape of HIV response is far from clear and remains uncertain. As of the writing of this policy brief, the United States has halted its President’s Emergency Plan for AIDS Relief (PEPFAR) for 90 days, along with other foreign aid in HIV and related responses, which has had an immediate impact on people living with HIV. This program provides funding for life-saving HIV medications across the globe, including in the Philippines. This is daunting, especially for those in the community working toward ending HIV, because their hard work over the past decades may be jeopardized, as experts predict that this lack of resources for the HIV response could mean a resurgence of the HIV pandemic.
We also believe that every challenge comes with opportunities. This current move by the United States can be seen as an opportunity for Australia to lead its allies and partners in the Asia Pacific Region and in the Philippines. However, we also recognise that the positive impact of this funding may be less felt, or not felt at all, by the average Filipino men who have sex with men, as we believe that funding agencies tend to be red-taped, meaning that funding undergoes numerous processes before resources reach the communities affected by these health conditions. To mitigate this and ensure a broader reach to the community, funding institutions, such as the Australian government, must decentralize their processes to make their resources much more accessible to those in need. It is time for Australia, as a nation, to extend its leadership to its allies within the Asia Pacific Region and the Philippines.
CONCLUSION
Addressing health issues like HIV and mental health in Filipino gay and bisexual men and other men who have sex with men requires holistic approaches. We must move beyond viewing these health conditions as purely medical issues and consider how various political and structural factors have influenced their experiences. To create effective interventions for these men, policymakers and healthcare professionals must recognise their lived experiences and incorporate their experiential expertise in designing, informing, and developing diverse health services, policies, and interventions. This necessitates action from various institutions, including the Australian and Philippine governments, to improve policies and programs for the Philippines and the Asia-Pacific region.
